Image fusion software allows surgeons to take advantage of the rich information and higher quality of preoperative scans by combining them with intraoperative images. This is especially helpful for spine surgery, since elastic fusion software even matches images in which the position of the flexible spine differs in each scan. Image fusion can help surgeons make critical decisions about the procedure in the operating room.
Intraoperative scans are essential for giving the current picture of a patient’s condition at the time of surgery. Intraop images, however, often lack the clarity of diagnostic-quality, preoperative scans. Most surgeons have access to at least one if not multiple high-quality preop images that they’ve ordered themselves or the patient has brought from a referring physician.
Adding the rich information from these higher quality scans to intraoperative images gives surgeons access to more information. Coming from the technology sector, we know that more data leads to more informed decision-making. To put all of this information into one place to save time and effort, surgeons will need advanced image fusion software.
What is image fusion for surgery?
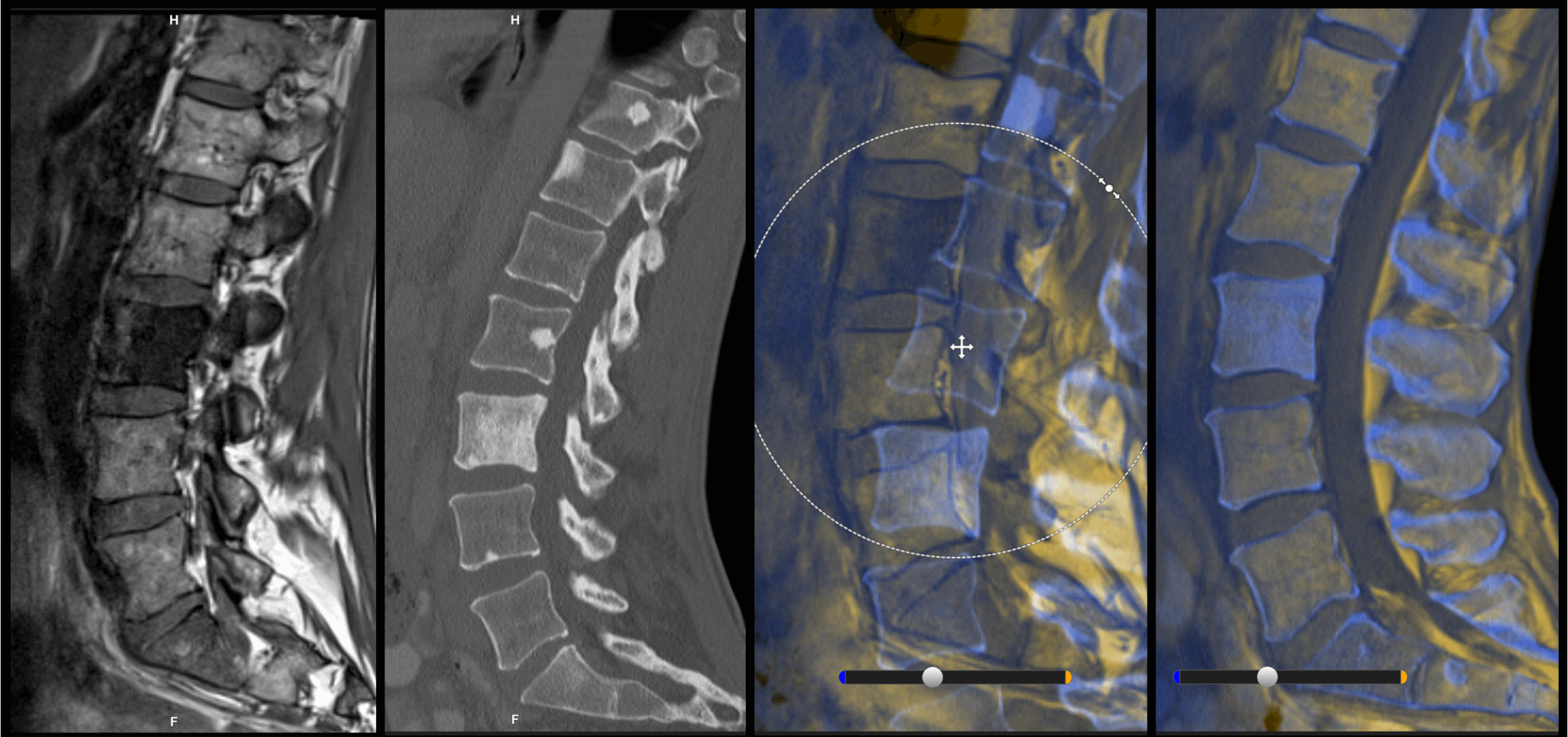
Image fusion allows surgeons to exploit all available anatomical and functional data simultaneously. This type of software combines CT scans, which deliver information about bony structures, and MRI datasets, which aid in soft tissue definition and tumor identification.
What is special about image fusion for spine surgery?
Identifying an issue that leads to spine surgery often requires larger, longer range scans. For example, a patient sees their general practitioner about persistent lower back pain. Before the GP can make a diagnosis, they will likely send the patient for an MRI or CT scan. This image usually covers a large portion of the spine to help with diagnosis. Fusing a relatively small intraop scan with the larger preop one gives surgeons a view into further spine levels and allows the surgeon to plan and outline during surgery.
Cranial fusion, unlike cranial surgery, is relatively straightforward. Bony landmarks of the skull allow for easy alignment of MRI and CT with rigid fusion. Due to the flexibility of the spine, however, there isn’t always a guarantee that the vertebrae will be in the exact same position in two different scans. That is why image fusion for spine surgery is more complicated than other areas of the body, requiring a method known as elastic fusion.
Rigid fusion versus elastic fusion for spine surgery
Rigid fusion is normally used when working on a few levels (2-4) and when the mobility or movement of the spine will not be enough to hinder navigation accuracy. A region of interest is manually selected and then a software algorithm will attempt to match the datasets.
Elastic fusion is a type of fusion that enables a dataset to morph. By morphing, it can compensate for a shift or change of position of the patient. An MRI, for example, would normally be taken with the patient lying on their back, while on the operating table for the surgery, they might be lying in a prone position. With elastic fusion, the MRI dataset is deformed to fit the position of the patient’s spine in their intraop position.
Why should surgeons be fusing images?
Today, more surgeons than ever have access to intraoperative imaging devices in their operating rooms. These include C-arms and iCT devices that can take images of varying quality. The tradeoff for most intraoperative image systems is that image quality is sacrificed for portability and convenience. Image fusion brings the higher quality of preoperative scans into the operating room.
Indeed, image fusion is all about making good use of something that surgeons already have: Preoperative images. An preop MRI, for example, can provide a host of additional anatomical information the surgeon may not have access to with their intraoperative imaging devices.
By fusing images together and registering them to the patient’s position, surgeons can navigate on both datasets and benefit from having all relevant information in one view. To learn more about image registration, please read our article “A Step-by-Step Guide to Image Registration for Spine Surgery”. With the corresponding software, surgeons can even navigate simultaneously on both sets of images, which in turn saves O.R. time.
Do surgeons who plan need image fusion?
Surgical planning is indispensable to ensuring that the actual result reflects the surgeon’s desires for the outcome. Understanding where they are headed and how to get there helps surgeons save time during surgery, especially in complex cases. The truth is, not all surgeries require planning. In some cases, in fact, surgical planning may add time during preparation that does not result in time saved during the procedure.
With the right software, image fusion can be completed in the operating room in a matter of seconds. This method instantly adds value from preop images and gives the surgeon seamless access to the fused images to make on-the-fly plans in the O.R.
Especially in the case of complex surgeries that do require a lot of planning, image fusion becomes all the more valuable. By adding in those preop images that the surgeon has carefully selected and studied, they are free to enter the procedure with the confidence that they have the most information at their fingertips in the operating room.
Image fusion is ultimately information fusion
Image fusion merges the information of preoperative images with the current surgical situation, offering surgeons the opportunity to make the most of the available data. Surgeons should take a look at the cases they are doing and the images they already work with to identify if image fusion would add value to their intraoperative decision-making.
For more on image fusion, including elastic image fusion, we recommend reading the Acta Neurochirurgica clinical paper “Augmented reality in intradural spinal tumor surgery”.